Platelet-rich plasma, or PRP, has emerged as a key component of regenerative medicine in orthopaedics. But despite its growing popularity, many patients still wonder: what is PRP therapy, and how does it actually help with joint and soft tissue conditions?
This guide aims to demystify PRP therapy, explaining what it is, how it works, and how it is used in orthopaedic care to support healing from injuries and degenerative conditions.
What Is Platelet-Rich Plasma?
Platelet-rich plasma is a concentration of platelets derived from your own blood. Platelets are small cell fragments that play a critical role in clotting and tissue repair. They’re also rich in growth factors—proteins that stimulate healing in bones, tendons, ligaments, and muscles.
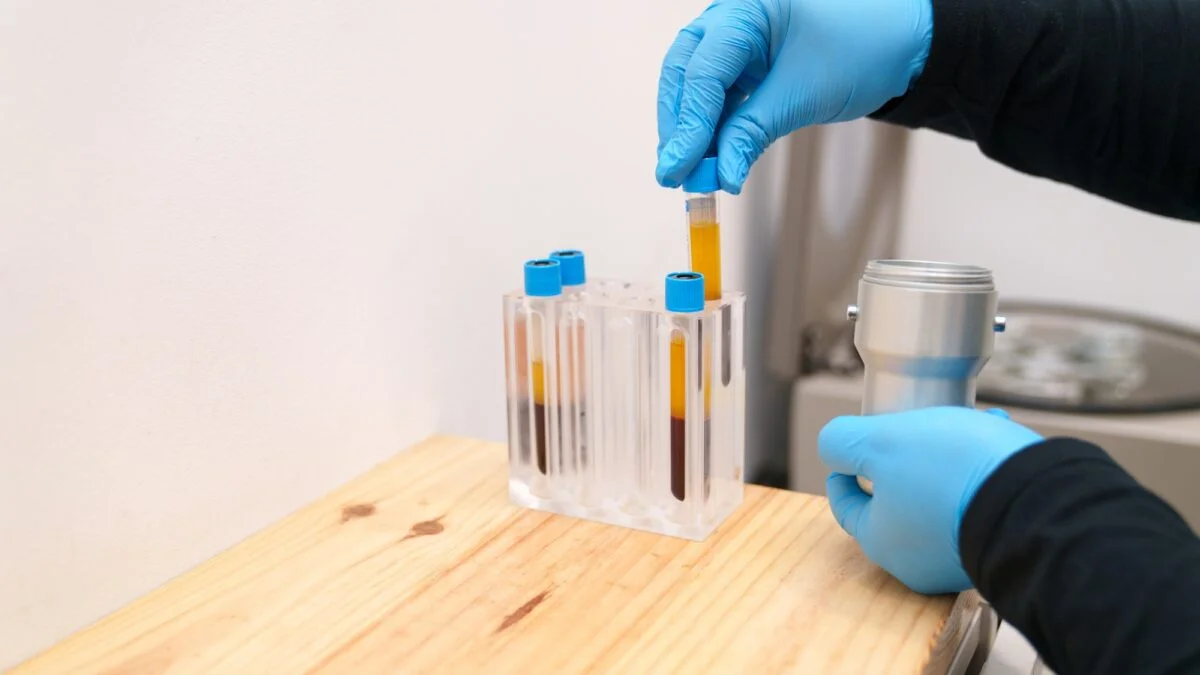
To create PRP, a small amount of blood is drawn and placed in a centrifuge. This machine spins the blood at high speed to separate the plasma and platelets from red and white blood cells. The resulting substance—platelet-rich plasma—is then injected into the area requiring treatment.
This process harnesses the body’s own healing capabilities, making it a natural option for managing orthopaedic injuries and degenerative conditions.
How Does PRP Work in Orthopaedics?
In orthopaedics, PRP injections are used to stimulate healing in damaged or inflamed tissue. When PRP is injected into an injured area, the growth factors signal the body to begin repair. This may help reduce inflammation, support tissue regeneration, and promote pain relief over time.
PRP is commonly used to treat:
- Joint degeneration – including PRP for knee arthritis, hip pain, and PRP for osteoarthritis
- Tendon injuries – such as PRP for rotator cuff injury, Achilles tendinopathy, and tennis elbow
- Ligament injuries – including PRP for ligament tears and joint instability
- Muscle strain and overuse – like PRP for muscle strain and sports-related injuries
- Chronic conditions – such as plantar fasciitis and shoulder tendonitis
Patients who haven’t responded well to traditional treatments often explore PRP as an alternative or complementary option.
What Conditions Does PRP Treat?
PRP therapy is used across a wide range of musculoskeletal concerns. It’s particularly helpful for conditions where healing is slow or incomplete due to limited blood supply or chronic overuse.
Common uses include:
- PRP for joints: knees, hips, shoulders, ankles
- PRP for tendons and ligaments: especially in areas that tend to degenerate over time
- Sports injuries: where regenerative medicine can support faster recovery
- PRP for back pain: in select cases involving facet joint inflammation or soft tissue damage
To see if your condition is suitable for PRP, consult with your provider for an accurate diagnosis and personalised plan.
Is PRP Therapy Safe?
Since PRP is derived from your own blood, the risk of adverse reaction is minimal. The procedure is performed under sterile conditions and often guided by ultrasound to ensure accurate placement.
Like any medical treatment, there are some considerations. Patients may experience mild swelling or soreness at the injection site. These effects are usually short-lived and manageable.For more on this topic, read our article on PRP therapy risks and benefits